Exploring opportunities through an idea generation workshop
We ran an idea generation workshop with NHS Digital stakeholders to come up with ways to improve the service.
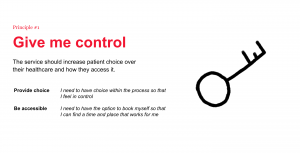
To ensure we were basing our ideas around user needs, we used the design principles, journey maps and user personas from the earlier research as a springboard for idea generation.
Doing this helped us to consider a range of needs and situations while we generated ideas.
For example, what would it look like to reassure someone at the point they compared appointment options? How could we adapt to their needs while they were waiting for their appointment?
We identified several key questions that arose from the ideas generated that we needed to test. These were:
- Would using SMS be useful?
- Could parts of the process be automated while still meeting users’ needs?
- Could we make the recorded menu easier to navigate?
In the next phase of the project, we developed prototypes that would help us test those assumptions.
Testing designs across diverse perspectives
We needed to test the service with people with different access needs, including disabled people, people with limited English, and people with low digital skills or limited access to technology. We also recruited people from communities who are more likely to experience health inequalities, including people from Pakistani, Bangladeshi and Traveller communities.
We used different mediums for our prototypes to cater to these different needs.
- A visual storyboard, to help communicate the context of what we were testing with people with limited English
- Mock-ups of SMS messages
- Audio recordings to test pre-recorded or automated parts of the phone line
- Text versions of the visual and audio prototypes so that users with low vision or hearing could interact with them
We also spoke to 3 GPs to understand the wider context of the service.
Keeping participants safe
Experiences with the health system can be emotional and for some people they can be traumatic. We wanted to be careful that our research wouldn’t cause people harm by asking them to re-live painful experiences. We were also mindful that there’s an unequal power dynamic between patients and their GPs, and that people might be worried that this research might affect their healthcare in some way. It was also possible that this research might affect us as researchers if it triggered painful memories of our own experiences.
To reduce the risk of unintentional harm, the team ran a session on trauma informed research where we reflected on these risks. As a result, we adapted our discussion guide so that participants could avoid talking about their own experiences, and provided follow up support resources. We also made sure we worked in pairs and checked in with each other after research sessions to look after our own wellbeing.
Analysing the findings
After analysing the findings from our research sessions, we found significant patterns that showed us whether the concepts were likely to work, and what would need to be taken into account for them to be successful.
For example, we found that SMS were useful, but should be used in combination with other channels which are perceived as more trustworthy. It also presented us with new needs, such as the importance for some people of choosing the gender of their clinician.
From design to procurement
We translated the findings into user stories – short descriptions of the required functionality from a user’s perspective. For example:
“As a patient or carer, I want to be able to call the service at a time that suits me.”
We used these to populate a service blueprint, which showed the user stories in the context of the user journey. The blueprint also contained the technical and operational capabilities that would be needed to fulfil the user stories. It clearly documents the high level design of the service.
To further support the procurement, we documented the user stories in a spreadsheet prioritised into ‘must have’, ‘should have’ or ‘could have’. This made it possible to directly assess whether potential suppliers met each requirement.
We also engaged with clinical safety, technical architecture, cyber security and information governance to identify and mitigate any risks that the service might pose to patient’s health or privacy. This included considerations such as workflows for call handlers to get consent and check contact information before confirmation messages are sent.
Including the planet as a stakeholder
At Snook, we’ve been working on ways to make sure we consider the environmental impact of the services we design. On this project, we appointed a team member to be a Climate Ambassador, the person responsible for making sure we considered sustainability throughout the project. We worked with a Sustainability Officer at NHSD to understand their climate strategy, and to identify how this service could help them meet their emissions reductions targets. This gave us a fascinating picture of the overall system impact a phone line could have. For example, by signposting people to public transport options to travel to their appointment, we could reduce emissions around hospitals and free up space for emergency vehicles.
We built this insight into the service blueprint, including a row for sustainability impact and highlighting where the service might increase or reduce emissions. For example, where paper letters could be replaced with emails or SMS messages.
An assisted digital service: clear, tested requirements of what to procure
By the end of the project, NHSD had a detailed picture of what they needed to procure to meet the needs of users, and a clear way to communicate this to the market. They had evidence to back up their decision making process and confidence they were procuring the right thing.
Our work provided a set of requirements the service must meet to ensure that all patients can book and manage their appointments, regardless of their access needs. We also suggested innovations to run the service more efficiently, backed up with data about the call volumes this might affect, and the findings from user research to take into consideration.
Finally, we provided recommendations for areas where NHSD could improve the wider service beyond the scope of the telephone line, and better meet users’ needs across all channels.
Our work will be directly used within the procurement of the future service to ensure it is accessible, inclusive and operated efficiently.