Systems re-design in eye care services
Creating a view of the whole eye care system and co-designing a future system in collaboration with Integrated Care Systems (ICS) across England
Taking a systems thinking approach to identifying problems in eye care
NHS England eye care services are facing significant challenges meeting patient demand and have been exasperated by the Covid-19 pandemic. A third of people are waiting in excess of 18 weeks to access eye care services in England, with more than 26,000 waiting more than a year. This means that due to lack of timely access to the right care people are losing their sight.
Partners across the NHS came together to respond to the backlog of patients requiring eye care services and to re-organise the system with the aim of increasing capacity and ensuring demand is met more efficiently at all levels.
“Ophthalmology is the busiest outpatient speciality in the NHS, with over half a million patients in England waiting for treatment as of April 2022”
So, what is an ‘eye care system’? It is the set of elements related to eye care working together as an interconnected network. There were lots of individual projects set up to improve eye care services – what was missing was an understanding of how eye care services fitted together, and if these projects would successfully resolve all the problems across the system.
In the first phase of this project we:
- Created a view of the whole eye care system
- Mapped out pathways for three sub-specialities from eye care professionals’ understanding
- Directed further research and re-design by identifying prioritised pain points and opportunities
Mapping
During the mapping process we first focused on reviewing previous research around eye care, drawing out relevant information to help us understand the current eye care system and its challenges.
We then spoke to people from across eye care services in England to gain a clearer understanding of, and map, the systems structure including the relationships and influence between different actors in the system.
Talking to people in different roles across the system enabled us to map the journey of three sub-speciality pathways. We held validation workshops to refine the journeys and to identify the pain points and opportunities.
Analysing the problems
We gathered and synthesised all pain points and opportunities across the maps to create problem statements then ran a workshop with stakeholders to organise them into 8 core problems affecting the eye care system and build consensus on the key opportunities to take forward into the re-design phase.
We conducted root cause analysis to understand the problems more clearly. The visual below illustrates how problems in the system were interconnected and that the root cause is very rarely one thing.
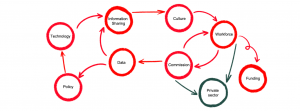
Figure 1: A visual of interconnected problems
Redesigning the system from the perspective of an ICS
We also created causal maps to visualise this which enabled us to distinguish between ICS and national problems and spot patterns between the problems, such as common root causes.
Working with one ICS we created a ‘Vision for the Future’ of eye care services. We used a theory of change framework to identify the short- and medium-term outcomes that needed to be achieved to deliver the vision. This was used as an anchor for the re-design work.
We also held a series of ideation workshops with representatives from the ICS’ eye care services around how eye care services should operate in the future and ways to address problems.
A list of key ideas were explored further with stakeholders to identify projects which reflected national, regional and local interests ready for testing.
Co-designing the future eye care system for all ICS’
Through the previous phase of work we had some concrete ideas for transforming a system from the perspective of one ICS, but with each ICS in England uniquely configured around their local landscape and specific needs of their local population, it was important to involve a broader range of ICS’ to design the new eye care system.
We delivered a series of bespoke workshops for different types of ICS’ across their local eye care services to stimulate conversations around the future of eye care in their area.
There wasn’t a ‘one-size fits all’ design and our role was focused on building consensus on the elements of the future eye care system across all ICS’ as well as identifying where local variations were required and why.
Different options for how the model could be deployed at an ICS’ level were then identified. Our conversations with ICS’ helped us validate and articulate the reasons why each option would suit different types of ICS’.
Developing an understanding of common elements of the eye care system established the role national eye care services could play in addressing blocks in the system and enable the changes to be delivered at a local level.
We continued our visual skills throughout this phase to help communicate key concepts and the final design. This included:
- mapping to key parts of the model along a high-level patient journey
- a theory of change diagram to explain the relationships between key elements of the model and how they will deliver the intended outcomes
- a systems view

Testing the design and building an evidence phase
Our final deliverable outlined recommendations for the next phase of the project. The team are planning to work with engaged ICS’ to test parts of the model with patients and eye care professionals and develop learnings. This will enable the team and ICS’ to validate assumptions in the design and build an evidence base for further investment to scale new ways to deliver eye care services to better meet the needs of patients and staff.
Learnings and reflections
Learn to sit with ambiguity
The size and interconnectedness of a system can be overwhelming. Re-frame the thinking here – use it to understand constraints, what can change now and what should be considered in the future.
It’s not about pretty maps
The value isn’t making the most beautiful map of a system. Decide what maps to make and how they add value to the narrative, or the alignment being attempted. No map works for everyone, so don’t try to make it.
Design for the root problem, not the symptom
Being met with ‘we already knew this was a problem’ can be disheartening to hear however this is a sign of being on the right track. People in a system are experts in their own experience. The challenge is to be sure to focus on the root of the problem, agreeing to solve those, and not get bogged down in the symptoms which people usually experience. The value of this work is the alignment built between people around the problems to solve.
Interested in learning more?
Join us on the User Centred Systems Thinking course
“It’s a balance of systems thinking without getting overwhelmed and detailed frontline design without getting tunnel vision. Get the zoom in and out right to be able to design for what’s directly in front and what we’re hoping for in the future.”